11/08/2020
Protecting the vulnerable against infectious diseases
Residential care homes and units for supported living are facing a very difficult situation in the face of the Covid-19 pandemic. Generally, care home inhabitants are the most vulnerable to the virus, and care homes have very limited resources to provide their customers with enough protection against the spread of infectious diseases. This article discusses possible mitigation actions, drawing on knowledge from the pharma and biotech industry.
We can only observe risks that we are aware of. To put it slightly harshly, crises tend to help identify risks at a general level. In several countries, residential care homes have reported unfortunate events of how the corona virus has caused devastation among their inhabitants, killing many defenceless, sick and elderly people. Thus, in the aftermath of this ongoing crisis, the authorities will most probably impose new controls to prevent the spread of infectious diseases in care homes.
Spreading paths
Many infectious diseases are airborne, which means that they spread via human respiratory organs. Viruses are insidious; they cannot be felt or seen in any way. To make matters worse, symptom-free persons can spread them.
To most people, the current disease has mostly been a (frightening) nuisance, but especially for elderly people it is a matter of life and death. The virus is generally brought into care homes by personnel who got infected outside of the care home, or by new inhabitants that come into contact with the other inhabitants. The main enabler is that the person in question has not yet developed symptoms of the disease. In these cases, the risks have not been properly identified.
Prevention or protection?
Having identified a risk, it should, if possible, be prevented. If this is not possible, the risk should be reduced to an acceptable level. In theory, preventing an infectious disease from spreading is very simple; the virus or all interactions between people must just be eliminated. In practice, this is, however, not feasible, so another strategy needs to be applied.
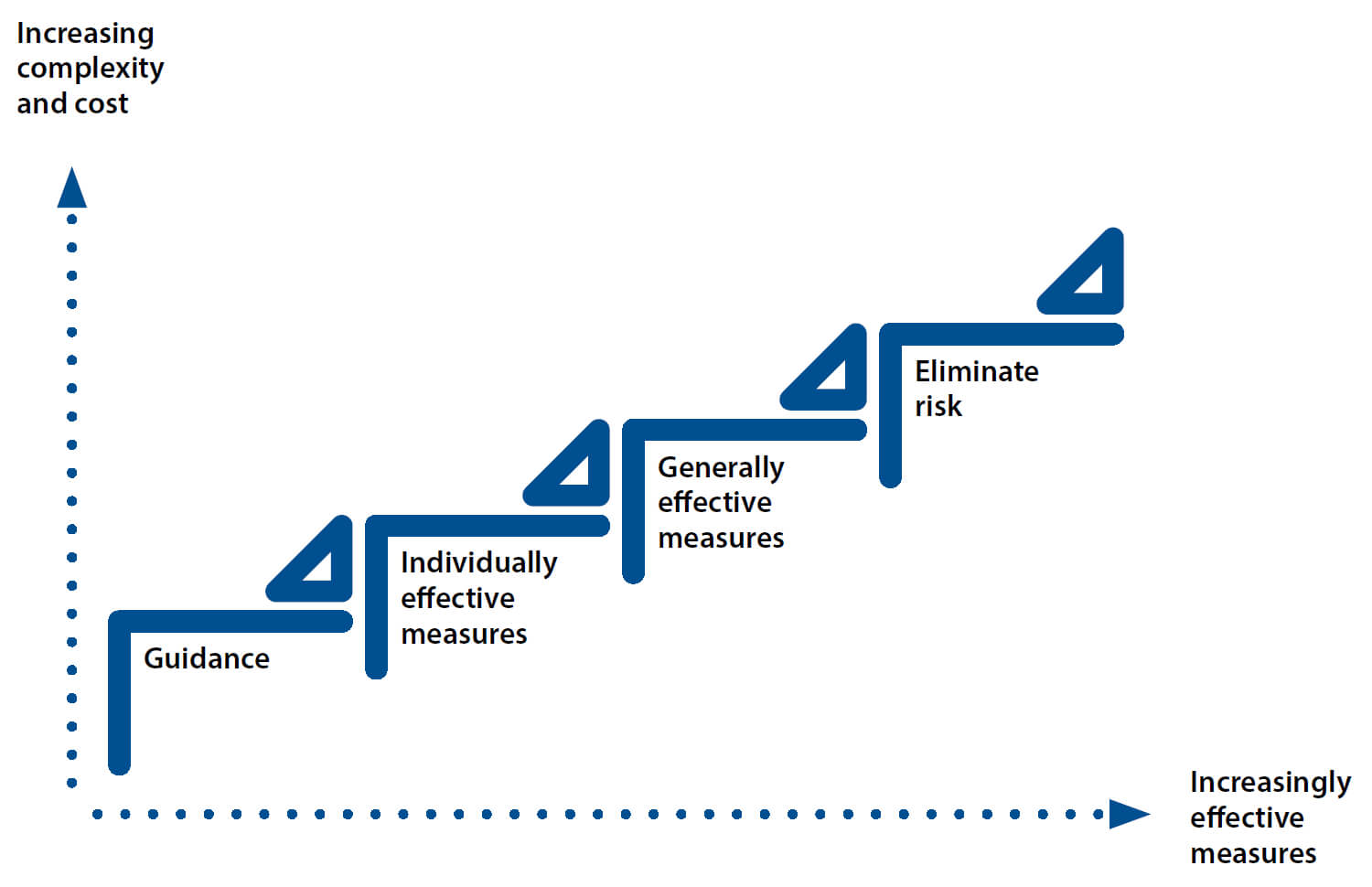
Risk reduction measures should be prioritized so that generally effective measures are preferred over personally effective measures, which in turn have priority over guidance only, which is the last step – and the least effective measure.
The availability of options boils down to cost and preparedness. Cost and timing are crucially important. In the face of a crisis, the mitigation measures at the lower end of the priority scale are in general the cheapest and quickest to implement.
When mitigating the spread of an infectious disease, the actions that are the simplest to implement are washing hands and wearing respiratory/face protection. They are also part of the least effective protective measures.
The more prepared one is, the larger the selection of available actions is. For example, if a facility was originally designed to enable quarantining or isolation of persons, and the personnel have been trained properly in dealing with infectious diseases, the best preparedness possible has been achieved. This is rarely the case, however.
Effective mitigation measures
As previously indicated, implementing a quarantine or isolation area is the most effective way of preventing the spread of disease. Currently, only few residential care homes and hospital bed departments have fully-fledged areas for the purpose. There are, nevertheless, some technical and organisational measures that can be implemented to reduce the probability of an outbreak. These measures can be selected by means of a risk-based approach.
‘Contamination’ and ‘crosscontamination’ are terms that are used in the pharma and biotech industry to describe the transfer of a contaminant into a product or carry-over of one product into another. These unwanted phenomena happen via various flows, which could be called spreading paths in this context. The idea is to cut as many spreading paths and flows as reasonably possible – or at least to ensure a unidirectional flow towards the quarantine/isolation area.
The risk-based approach mentioned above would include identifying all possible spreading paths, assess their importance with regard to possible transmission, and develop effective mitigation measures to cut as many paths as possible from a technical and economical perspective.
This systematic, in-depth study then presents the possibilities available and modifications required at the facility. Typical paths may be related to persons (inhabitants and personnel), materials (e.g. foodstuffs, mobility aids) and air (both building ventilation and exhalation). The target is to keep “wildcards” separated as much as possible from the rest of the inhabitants and personnel. Some level of added safety can sometimes be achieved relatively simply by e.g. closing a door or two inside the facility and using a back door as a spare entrance. If ventilation can be separated for a certain area, that could also increase safety.
Organisational measures are generally as important as technical ones. Especially when there are people who have fallen ill, preventing personnel exchange between departments is crucial. One way to do this would be to provide a “takeaway” meal service to the quarantine or isolation ward. There are many aspects that can and need to be observed, and in some cases professional advice may be beneficial. The most important perspective, however, is to ensure that everyone is provided human interaction and care.
Return on investment
How does one calculate the return on investment (ROI) for an investment that is not directly related to increasing the accommodation capacity of the facility? How does one quantify the value of possibly being able to save human lives? To be able to answer this question, one needs to consider business dynamics. Competition always favours the prepared and good business reputation is founded on preparedness.
The recent events caused by the corona virus pandemic will certainly have at least two consequences: firstly, the authorities will most probably introduce legislation that obliges care home operators to identify and address risks related to infectious diseases, and secondly – and more importantly – customers and their families will question whether their elderly family members are safeguarded against diseases in a facility.
Therefore, if a facility is safe, customers will come knocking at its door also in the future. This is a clear return on investment that will also allow carers to safely focus on their core business.